CHAPTERS
Navigate to chapter
► Chapter 1: Age 0-6 Months, Breast Milk or Formula
► Chapter 2: Age 6 Months – Introducing Solid Foods
► Chapter 3: Your Child’s Nutritional Needs
► Chapter 4: 12 to 24 Months
Chapter 1: Age 0-6 Months, Breast Milk or Formula
Expectant parents work hard at the pre-planning stage of having a baby. Some opt to know the gender of their child so they can buy all the right things and decorate accordingly.
Amid all that preparation, most parents make carefully considered decisions about how they plan to feed their child — only to be brought up short when circumstances completely out of their control demand another approach.
It’s perfectly fine to prepare to breastfeed (completely or in part) or to bottle feed, but allow yourself a window of opportunity to change your mind if you need to.
If you haven’t made the decision between feeding breast milk or formula to your baby, we need to discuss the major considerations for both nutritional approaches.
Deciding to Breastfeed
There are many well-documented reasons to opt to breastfeed your child. A mother’s milk is full of antibodies that will help her child fight off diseases. Researchers even believe that breastfed children are at a lower risk for Sudden Infant Death Syndrome (SIDS).
The antibodies naturally present in breast milk protect against such problems as:
- chronic ear infections
- stomach viruses
- asthmaand respiratory infections
- diabetes (Type 1 and 2)
- childhood leukemia
Studies also indicate that breastfed children are at a lower risk for the development of obesity over their lifetime.
Interestingly, the benefits are felt by the mother as well. Mothers who breast feed show a decreased risk for developing breast and ovarian cancers, struggle less with postpartum depression, and gain protection against diabetes.
Typically, babies digest breast milk more easily. Some commercial formulas are made from cow’s milk (albeit low fat cow’s milk), which contains proteins infants may have difficulty tolerating at first.
That being said, there are a number of advantages to formula feeding:
- The ability to monitor exactly how much the child is eating.
- Shielding the infant from side effects from any foods the mother is eating, illnesses she experiences, or medications she requires.
- Allowing all members of the family to participate in feedings, facilitating more bonding time with both parents and siblings.
Since babies eat slightly less often when fed formula, the number of feedings per day decreases somewhat, which may better match some family’s schedules.
Considering the Middle Ground
Some people fail to realize that there is a middle ground position, partial breastfeeding. This is not an all or nothing proposition.
Partial breastfeeding works especially well for mothers who are having difficulty producing enough milk and for working mothers who simply cannot find the time they need to breastfeed or to express milk.
There is no set rule for deciding how much breast milk your child receives opposed to the baby’s intake of formula. Advocates of breastfeeding are universal in saying some breast milk is always better than none.
If you are considering partial breast feeding, mitigating factors to consider might include such things as:
- the working schedule of one or both parents
- how much breast milk can be successfully expressed and stored on a regular basis
- the quantity of milk you are actually able to produce
It is generally recommended, however, that if at all possible the child receive four weeks of exclusive breastfeeding before any formula is introduced.
Myths and Misconceptions About Breastfeeding
Often our beliefs about any topic, especially one as emotionally charged as breastfeeding, are deeply influenced by the opinions that are dominant in our culture — even if those ideas are actually myths.
Inadequate Milk Production?
The idea that many women cannot produce enough milk is certainly a misconception. Actually, the exact opposite tends to be true.
In cases where a child does not thrive on breastfeeding the real problem is almost always that the infant is poorly latched on. All mothers, but especially first time mothers, need instruction in helping their child breastfeed.
Women have been breastfeeding babies for centuries, but that doesn’t mean that either the mother or the child know exactly what to do automatically.
Lactation specialists and trainers can help enormously by simply observing a feeding and offering helpful instruction. This kind of training is typically available at the hospital where the child is delivered.
Modern Women Can’t Produce Milk?
You will likely hear the absurd notion that modern women are no longer capable of nourishing their children exclusively from breast milk, or that an inability to produce adequate milk is an inherited trait. Neither of those “facts” is true either.
Humans are mammals. We are biologically designed to produce milk for our young. Problems with nursing can often be resolved by something as simple as nursing more frequently to stimulate production, offering both breasts during feeding, or massaging the breast gently while the child is suckling.
Breast Feeding is a Choice
In the midst of all this information, however, please don’t lose sight of the fact that breastfeeding your baby is a choice. It has to work for you as well as for the child.
It’s far too easy for a new mother to be shamed into breast feeding by doctors, nurses, family, and well-meaning friends. The truth is that some women just do not like to breast feed. That is perfectly fine.
There is no imperative to breast feed in order to qualify as a “perfect” mother. Your child will certainly know if you’re uncomfortable or unhappy during feedings.
The optimal situation for you both is the one with the least amount of stress and the greatest amount of calm bonding time. If you are worried that formula will not meet your child’s nutritional needs, there really is no need for that groundless fear to rule your decision.
How-To: Breastfeeding Basics
Although many first-time mothers find it helpful to watch breast-feeding “how to” videos or to work with a lactation coach, these are the basics of positioning your child to latch on to the nipple for feeding.
Step One:
Find a comfortable location. Feeding times can vary significantly from 5-40 minutes. You want some place that is quiet with no distractions, especially in the beginning.
As you become more accustomed to feeding your child, you will be able to quietly read or listen to music through your headphones without upsetting your baby or disrupting the feeding time.
Step Two:
You can lie on your back to breast feed with your baby resting against your body, or cradle the child across your chest.
Have pillows or cushions ready if you are holding the child and your arm begins to tire. Make sure your back is well supported.
Step Three:
Bring the child to your breast with the head tipped back so that the baby is leading the motion with its chin. When the child’s lips touch the nipple, the infant will instinctively drop the lower jaw. With a smooth, quick motion move the baby’s mouth on to the breast.
Pay attention to the sensation when your child takes the nipple. In latching on, the child should take a mouthful of tissue.
To ensure this is the case, the child’s mouth should be wide open as it comes on the breast. Remember, the child’s tongue, bottom lip, and chin makes initial contact. The bottom lip should be as far from the base of the nipple as possible.
If you experience pain, the baby is not latched on correctly. If this is the case, place your finger gently between your child’s mouth and your breast to break the seal and begin again.
Don’t just carry on in a state of discomfort or your nipples will become too sore to properly feed your child.
You will know that the feeding is going well if the child progresses from short, quick sucks to slow, deep suckling. The child’s head should be tipped back with the chin touching the breast with the nose free and clear.
There should be more of your areola visible above the child’s upper lip than below the bottom one.
Step Four:
Allow your child to nurse for as long as the baby is hungry. The child should be relaxed and content, not wriggling around. The infant will release the breast when they are done.
Step Five:
At the end of the feeding examine your nipple. If it appears “squashed,” it’s likely it was not far enough back in the baby’s mouth and you still need to improve the child’s ability to latch on well.
The nipple should be at the back of the child’s mouth where the hard palate ends. The child’s jaw will move up and down with the action of the tongue to draw the milk into the mouth. The baby’s lower gum should never touch the breast.
Additional Tips:
Place your palm behind the child’s shoulders and your index finger and thumb behind the ears to support the head and better direct the baby’s motion toward the breast.
If the child’s hands are in the way, try wrapping the infant in a blanket so the baby’s arms are at the sides. This will let you keep the baby closer to the breast for more successful feedings.
Keep your hand away from your nipple as much as possible. Once the baby is properly supported and nursing, stay as still as you can.
When your child is sick, breastfeeding will supply needed comfort as well as nutrition and can help to settle a fussy baby.
How-To: Store Breast Milk
Before handling breast milk, always wash your hands thoroughly with soap and water. Breast milk should be stored in glass or hard plastic containers.
There are special bags designed for milk collection and storage that may also be a good option, however, bags are not ideal for long-term storage due to the potential for leaks and breakage.
Be sure to label each container of milk with the date it was expressed. If the stored milk is to be taken to another site, be sure the label also includes your child’s name.
Always store breast milk at the back of the refrigerator where the temperature will be at its coolest. Try to put just enough milk in each container for one feeding so there will be less waste.
A good starting point is 2-4 ounces (59-118 milliliters). You can adjust the amount as you become more familiar with your baby’s feeding habits. It’s always a good idea to store some smaller portions for irregular feedings.
It’s alright to add additional milk to a portion that was expressed earlier in the day so long as the extra amount is allowed to cool completely.
Freshly expressed breast milk will keep at room temperature, (not to exceed 77°F / 25°C), for up to eight days in the refrigerator (at 32° – 39°F / 0° – 3.9°C) or in a cooler with ice packs for up to 24 hours. You can also freeze your breast milk for up to two weeks.
Make sure to leave a bit of room at the top of the bottle for expansion during freezing. Thaw your frozen milk by moving it to the refrigerator. It will take approximately 24 hours to thaw your milk.
If you plan to use the milk immediately, make sure to run warm water over the bag or bottle until it reaches room temperature. Never refreeze your breast milk.
Selecting Nursing Pads
It’s almost impossible for a breastfeeding mother to predict when or if she’ll “leak.” Having at least a package of nursing pads on hand is an excellent idea until you know more about how your body will function while producing milk.
Nursing pads can be purchased that are disposable or washable. You may actually want both. When you’re away from home having disposable pads makes more sense, especially since you will always want a dry, clean pad on hand.
Airflow and absorbency are major considerations. Pick pads that are 100% cotton. Disposable pads should have multiple layers for maximum absorbency, but avoid plastic liners unless they are “breathable.”
Don’t use liquid fabric softener with reusable pads, or they won’t take in as much liquid. Always remember that using a wet pad or one with poor airflow increases the risk of yeast infections. Always discard wet pads and put fresh ones in place as soon as possible.
Bigger pads are more discreet under clothing, and pads that are pink will be less visible. Disposable pads have the advantage of adhesive backings to help them stay securely in place.
Buying Nursing Bras
Women are used to the idea that their regular clothes won’t fit as their pregnancy progresses, but many aren’t prepared for requiring new lingerie. By at least the 16th week of the pregnancy, your bra will no longer be sufficient to support your breasts.
By the second trimester, you will likely need to be fitted for new bras yet again, and by the final weeks of your pregnancy you’ll want to have your nursing bras purchased.
Shopping at a maternity shop is the best way to get the right advice on fit and materials. These stores have fitters trained in helping pregnant women. Just increasing the size of your regular fashion bra will not work and will likely increase your level of discomfort.
The cups of a nursing bra provide access to the breast for your baby. You want to make sure that you can open the flap one-handed, so pay particular attention to the type of closure. Select bras that are 100% cotton or a breathable cotton or Lycra blend.
While it may be tempting to scrimp on the cost of your nursing bra based on the reasoning that you won’t be using it for long, don’t give in to that type of thinking. Get a good, quality bra that won’t place pressure on your milk ducts increasing the chance of a blockage.
For this reason, lactation specialists are against nursing bras with underwires. If you are used to an underwire, find a nursing bra with a flexible plastic underwire, but have another bra on hand without the wire insert in case the wire does prove to be uncomfortable over time.
Buying Breast Pumps
Breast pumps are typically recommended in the beginning to increase milk production. A pump can be an excellent tool, but it isn’t always necessary.
Many women do choose to pump even when their child is feeding well simply to reinforce the “message” to their breasts. The best strategy, however, is the one that fits your goals.
You can use a pump for a few weeks to maximize production, or to have breast milk on hand for your child when you can’t be present for feedings.
Choosing a pump can be a difficult decision, especially for new mothers. Hospital grade pumps, although too expensive to purchase at $700-$1500 / £432 – £925 are the most efficient.
These units can be rented for $40-$80 / £25 – £50 a month and are used with personal attachment kits that are purchased separately. The major manufacturers of this class of device are Ameda and Medela.
Consumer grade electric pumps are single user and come in a variety of capacities. On the higher end, these units have dual pumping settings at full suction, and can be highly effective. These units are priced in the $150-$350 / £93 – £216 range.
A good pump is one with a strong mix of suction, strength, and cycling speed. If a pump reaches full pressure too quickly, for instance, it can cause tissue damage, but so can a unit that builds its suction too slowly.
Overall, experts agree that renting a hospital grade pump is the best option. The smaller, less expensive pumps wear out or break down, and they don’t draw milk out efficiently.
In many cases, an older manual pump can be more effective than a brand new, but low-quality electric pump. Since the rule is always to get the best tool you can afford, the best in this case is a rented hospital grade pump.
You will likely have to experiment with multiple flange sizes as friction will cause soreness, as will allowing the pump to take in too much tissue. The majority of women do well with a 27-29 mm flange.
It is even possible to use the oldest method of extracting milk, hand expression, which is an art that comes quite naturally to some women. If this traditional methods works for you, it should be performed with the same frequency and duration as with a mechanical pump.
Regardless, you should pump both breasts simultaneously to get the greatest volume. Nurse your child for as long as the baby will eat, and then pump.
When to Stop Breastfeeding
There are no set rules about when to stop breastfeeding. Mothers who make the decision to continue offering their child breast milk into the second year of life may have to deal with social criticism, but the truth is that medical science does come down in their favor.
Breastfeeding lowers the risk of many childhood diseases, and also mitigates the long-term risks of cardiovascular disease, diabetes, and degenerative disorders of the nervous system like multiple sclerosis.
Breast fed children are more slender, have better vision, experience fewer ear infections, and have stronger dental health. They have better digestion with less vomiting, acid reflux, and constipation and have a stronger immune system.
A child’s brain triples in size from birth to age two. Breast milk contains omega-3 fatty acids, in particular DHA, which enhances brain development.
The World Health Organization actually recommends that mothers feed their children up to age three! So, bottom line, if it’s working for you and your child, breastfeed until YOU think it’s time to stop.
Formula Isn’t “Second Rate” Nutrition
While breast milk is optimal, modern day baby formulas are not second rate nutrition. These products are themselves based on the nutrient values and levels found in breast milk.
Over the last two decades there has been tremendous pressure placed on women to breast feed, but studies conducted in 2012 found that setting achievable goals is much more realistic and beneficial — even if only partial breast feeding is possible.
In part, the high nutritional quality of currently available baby formula influenced the outcome of these findings. “Judgments” of both formula and breast milk are far more relative than once believed.
Researchers are now more directly confronting the fact that breast milk itself is far from “standard” in composition and can even vary in “quality” from one feeding to the next.
For instance, the amount of fat in breast milk is affected by the mother’s daily intake. Any nutritional deficiency present in the mother will be reflected in her milk.
A baby’s changing nutritional requirements must also be considered. At four months, your child’s need for iron increases sharply. Breast milk alone can no longer meet that requirement, nor will a mother’s milk provide the necessary levels of Vitamin D.
By six months, babies need greater amounts of protein. Regardless of the level of milk production of which the mother is capable, other food sources will need to be added to the child’s diet at this time.
When you encounter recommendations for exclusive breastfeeding like those offered by the World Health Organization, it’s important to remember that those goals are directed primarily toward mothers in underdeveloped nations with poor sanitation and hygienic.
In those environments, breast milk is crucial in improving a child’s immune system and protecting against disease. These considerations do not necessarily apply in the developed world.
Putting Formula in Perspective
A hundred years ago when mothers could not nurse their babies, the services of a wet nurse were essential for the child’s survival. Infant mortality rates were high because not everyone could afford to hire a nurse.
In the latter half of the 19th century this nutritional gap began to be addressed with baby formulas based on cow’s milk. Justin von Liebig developed the first commercial formula in 1867, “Liebig’s Soluble Food for Babies.”
Over the next few years the recipes for these formulas included cow’s milk, water, cream, sugar, and honey. The latter alone is cause for serious concern.
Honey should never be given to children under one year of age because it contains the spores that cause botulism. The consequences of this exposure can be fatal to infants.
The emphasis in the recipes for these early formulas was based primarily on palatability. With high infant mortality rates in the absence of available wet nurses, the desire was to get children to eat – anything.
Apart from other real concerns, however, the fundamental problem with these first commercial formulas is the fact that they were based on cow’s milk. Human babies should never be fed whole cow’s milk.
Whole Cow’s Milk
Every species of mammal produces unique milk that is nutritionally tailored to the needs of that animal. A calf’s needs and those of a human infant are decidedly not the same.
Simply consider the rate of development in the two “babies.” Calves get up and start walking shortly after birth. Human babies come into the world at a much earlier and more vulnerable stage of growth.
Cow’s milk contains levels of protein that are too high for human infants. Whole milk should never be given to a baby under 12 months of age due to a risk of intestinal blood loss that can lead to anemia.
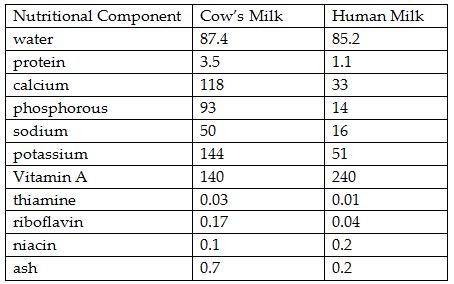
Additionally, cow’s milk contains 63% fatty acid content where breast milk has only 43%. Broken down in a comparison per 100 grams, this is how the two substances differ:
There are numerous additional considerations with cow’s milk:
- It forms large curds that digest slowly.
- The short chain fatty acids irritate the intestine.
- The high phosphorous content can cause convulsions.
- The level of ash leads to episodes of diarrhea.
- Qualitatively, cow’s milk does not provide a good supply of iron. It has a low level of Vitamin A, and almost no Vitamin Dunless it has been “fortified.”
Vitamin A deficiency causes blindness in infants, while there is a link between insufficient Vitamin D and autism.
The National Academy of Sciences Institute of Medicine doubled the recommended levels for vitamin D intake in 2008, so even human breast milk will no longer meet this nutritional need.
Modern Baby Formula
As scientists began to understand and appreciate the developmental benefits of breast milk, they refined the accepted recipes for infant formula significantly.
In the 1950s the first preparations using low-fat milk and vegetable oil were introduced, and more consideration was given to the quality of the proteins present in the milk used.
There are two categories of protein in milk, the casein faction and the whey faction. Casein is predominant in cow’s milk at a level of 80%, while human breast milk is 60% whey and 40% casein.
Ultra-filtered whey proteins were first introduced into infant formulas in the 1970s, beginning a process of refinement that resulted in the highly sophisticated products available today.
Given this progressive development using human breast milk, not cow’s milk as the nutritional gold standard, modern baby formulas will definitely give your child a good start in life even if no breast milk is available in the infant’s diet.
Regardless of the amount of formula you decide to incorporate into your child’s diet, you still have a huge hurdle before you – deciding which one to use!
Selecting a Baby Formula
While the whole breastfeeding vs. baby formula discussion may seem straightforward, when you walk into a store to purchase a baby formula, you may find yourself staring slack-jawed at the vast array of products.
Ignore Advertising Hype
Over the past decade there has been a tremendous amount of public controversy over product labels on infant formulas. The manufacturing companies can and do make all sorts of claims about the added nutritional value of their products – most of which are completely unsubstantiated.
What Not to Ignore
The statements regarding formula content that you do not want to ignore include:
iron fortified – If you are not breastfeeding your child, an iron-fortified formula is necessary for the baby’s growth and development.
enhanced with DHA and ARA – Some studies indicate that docosahaxaenoic acid and arachidonic acide, both essential omega-3 fatty acids, aid the development of your child’s brain and eyesight.
pre- and probiotics – These additives are intended to ensure the presence of healthy bacteria in the intestinal tract. Studies suggest positive long-term benefits, but you may want to discuss these foods with your doctor.
expiration date – Do not buy and never use a formula that is expired. There is no way to determine the quality of the product once the recommended date has passed.
Examine all containers for any dents or bulges. Look for leaks and/or rust spots. Don’t buy any formula in a container with these kinds of irregularities.
Four Major Types of Formula
There are four major types of baby formula currently available, which I will discuss below. Your first option will likely be a formula based on cow’s milk.
If your child is not tolerant of this type of product, however, there are other choices of which you should be aware.
Cow’s Milk
Formulas based on cow’s milk have been modified to replicate human breast milk as nearly as possible, both for nutrient content and digestibility.
These products should have the correct balance of protein, fat, and carbohydrates, and are designed to be as close to human breast milk as possible.
Soy Based
Soy-based formulas are an option for mothers who want their child’s diet to be free of animal proteins. These preparations are also used in children that are allergic to or intolerant of cow’s milk formulas.
Protein Hydrolysate
In protein hydrolysate formulas, the protein has been broken into smaller sizes than those present in cow’s milk or soy products.
This enhances ease of digestion, making these formulas the “last resort” for children who have proven intolerant of cow’s milk or soy-based formulas.
To further complicate the number of choices, formulas are available in three major form factors which I will discuss shortly.
Specialty Formulas
You will also see a plethora of “specialty” formulas, some for premature or “low birth weight” babies or those that are “metabolic” to deliver highly specialized nutrition.
Do not select a specialty formula for your child without consulting with your pediatrician. These formulas should only be given to your child for a specific medical reason.
Make sure that you understand that reason, and have clear recommendations from your doctor on the correct specialty formula to feed your child, as well as the amount of and frequency of feedings.
Typically, when specialty formulas are indicated, you will be closely monitoring food intake and the child’s weight and reporting these findings to your pediatrician.
The need for a specialty formula does not necessarily mean there is any serious health concern. Your baby may need more help to get over a case of colic, or to get relief from acid reflux.
Formula Product Formats
Infant formulas are available in three formats including powdered, concentrated liquids, and ready-to-use.
Powdered
Powdered infant formulas are the least expensive, but the most time consuming of all formulas. It is necessary to follow the preparation instructions exactly.
Many parents choose powdered formulas over concentrated liquids or ready-to-use varieties because the boxes do not contain bisphenol A (BPA), which is found in plastic containers and the lining of some cans.
In the body, BPA mimics estrogen and disrupts the endocrine system, which can harm brain and immune system development among other negative effects.
(Although powdered formulas circumvent the BPA worry, they do have to be mixed with water, which raises a whole new level of concern about toxicity. See the section below, “A Word on the Water Supply.”)
Concentrated Liquid
Concentrated liquid formulas are mixed with water (generally in equal parts). In terms of expense, these are the middle ground products. They are slightly easier to use than powdered formula.
Ready-to-Use
Ready-to-use formulas are the most expensive option – about 20% more costly by volume – but they are also the most convenient.
Hospitals rely on ready-to-use formulas not only for ease of feeding, but also because the products, which require no mixing, are hygienic.
If you live in an area where the quality of the water supply is questionable, or if you are not comfortable with the available water supply, ready-to-use formulas are your best option.
Note that once opened, a ready-to-use formula must be given to the child within 48 hours or discarded.
A Word on Water Supply
Since some infant formulas have to be mixed or diluted with water – and since your growing child needs water – you must seriously consider the fact that “plain” water may be one of the most dangerous things your child can encounter.
In August 2013, the Environmental Working Group released a report, “Water Treatment Contaminants: Toxic Trash in Drinking Water,” based on an analysis of samples taken from municipal water systems in 43 states in the United States.
Every one of the systems tested positive for chemicals the report labelled “probably human carcinogens.” The problem, however, is more sinister and extensive.
Chlorine, and other chemicals used to “treat” water to make it safe for human consumption interact with organic particles in the water supply.
These particles may be anything from cattle manure to animal carcasses to fallen leaves. The by-products of this interaction are highly toxic.
In theory, the chemicals disinfect the water, but the resulting “disinfection by-products” or “DBPs” are 1000 times more toxic than the decontaminants themselves.
At one time, chlorine was the primary additive in drinking water. Most treatment facilities, however, now use chloramine, which is a combination of chlorine and ammonia.
Chloramine cannot be removed from water by distilling, boiling, or outgassing (allowing the water to stand uncovered overnight.) Three of the disinfection by-products with which the report was most concerned are
- trihalomethanes– associated with bladder cancer as well as gestational and developmental problems in children
- volatile organiccompounds – which damage the central nervous system and irritate mucous membranes
- haloacetic acids– connected to liver disease, retardation of growth, low birth weight, neurological defects, and sperm toxicity
Some experts warn pregnant women against showering in water treated with chloramine because the disinfection by-products are absorbed through the skin.
This is all sufficiently frightening, however there is more. The report actually detected a total of 116,000 man-made chemicals in the municipal water supplies tested, including pharmaceuticals flushed into the sewers.
It is no easy matter to find chemical free water, since bottled water companies have been caught in the act of selling tap water and labelling it as “spring fed” or “all natural.”
Premium Bottles
So-called “premium” bottles mimic the natural shape of the human breast. They are made of polycarbonate, but are certified to be free of BPA.
Since the nipple is incorporated in the design of the bottle rather than a separate unit, premium bottles are easier to clean.
You will, however, be faced with changing premium bottles according to a scheme of “flow rate” according to four age steps: birth to 3 months, 3-6 months, 6-9 months, 9 or more months.
Stainless Steel
Stainless steel baby bottles are relatively new on the market. They are not inexpensive, but the material is believed by many to be cleaner and free of potentially toxic chemicals.
These hourglass shaped bottles are typically sold in sizes of 5-9 ounces / 148 – 266 mil with varying flow rates.
Buying Baby Bottles
Your first lesson in just how stubborn a baby can be may come when you buy what you regard to be the “perfect” baby bottle and your child hates it!
Bottles and nipples come in all sizes and styles, so be prepared to go through some experimentation before you find what your infant likes and will reliably use. The primary guiding factor in your selection really should be materials.
In July 2012 in the United States, the Food and Drug Administration banned the use of bisphenol A or “BPA” in baby bottles and “sippy” cups. (BPAs have been banned in Europe since March 2011.)
To make certain the product you are buying does not contain this chemical, don’t buy plastics marked with the number “7” or opt for old-fashioned glass bottles.
Bottle Types
In terms of shape and size, there are many types of baby bottles available, starting with the iconic “standard” and running the gamut to the newer aluminum bottle that looks like a baby thermos!
Standard
Standard bottles have the classic shape we all think about when we hear the phrase “baby bottle.” They typically hold 8-9 ounces, but can be found in a range of sizes from 4-11 ounces.
These bottles are easy to fill and hold. Most breast pumps and bottle warmers were designed with this shape of bottle in mind. Standard bottles are available in glass or plastic.
Angle Neck
Angle neck baby bottles facilitate being held at a 45 degree angle to allow milk to collect efficiently around the nipple. This means your child will swallow less air.
It’s also possible to feed your baby with one of these bottles in a slightly more upright position, reducing the chance of fluid collecting in the ear canals.
Most are outfitted with a vent in the base to help keep bubbles out of the mixture and to facilitate cleaning. The only drawback to the angle neck format is that it can be difficult to fill.
Wide Neck
Wide neck baby bottles are somewhat shorter and broader across than standard bottles. They are also available in plastic and glass. Supposedly a wider bottle feels more “breast-like” to the infant, and may be most appropriate for infants fed a combination of breast milk and formula.
Disposable Liner
These bottles are the middle ground between glass and plastic bottles. The outer shell is reusable, but the inner, pouch-like liner is discarded after each feeding.
The primary concern with these bottles is whether or not the liners are indeed free of BPAs. Although the liners, which collapse during the feeding, help to prevent your infant from ingesting air, they are also expensive over the long term.
Natural Flow
The design of these bottles is a two part central vent that acts like a straw. The idea is to eliminate the vacuum formed by the child’s suckling to prevent air bubbles from forming.
In theory, natural flow bottles reduce instances of colic and gas. The containers are available in both plastic and glass, but the straw attachment is difficult to clean without the included tiny brush.
How-To: Bottle Feeding Basics
It is recommended that you purchase glass baby bottles rather than plastic ones that may contain toxic bisphenol A and other chemicals that are released upon heating.
If you have never given a baby a bottle, you may want to find videos online or ask one of the nurses in the hospital to help you the first time you feed your baby.
Don’t forget to burp you baby after a feeding to bring up any air the infant might have swallowed.
Step One:
Take all new bottles and nipples and submerge them in boiling water for a minimum of five minutes, allowing the items to dry on a clean towel. After this initial sterilization, the items can subsequently be run through a normal dishwashing cycle for cleaning.
Step Two:
Mix the formula following the instructions on the packaging precisely.
Step Three:
Although there is no health-based rationale for heating formula, most babies prefer it if their bottles are placed in a bowl of warm water or simply under a stream a warm tap water. Never use boiling water or heat formula in the microwave.
Step Four:
Cradle the child in a partially upright position while supporting the baby’s head. It is important not to bottle feed a baby that is lying down. The formula can accidentally run into the middle ear and cause an infection.
Tilt the bottle so that the formula is in the neck of the container and covering the nipple
Expect your baby to take 2-4 ounces / 59 – 118.3 mil) during the first few weeks every 2-4 hours. Do not try to get your child to finish a bottle. Let the infant take as much as it wants and then stop.
Burping Your Baby
When babies gulp down either breast milk or formula, they also swallow air that collects in the esophagus, especially if the child is young enough to lie down most of the time. This causes gas, and also leads to the child spitting up its food.
Burping your child helps the baby to get rid of gas and hopefully to save off the regurgitation. For bottle fed babies, burp after the child has consumed 2-3 ounces / 59-89 mil). For breast fed children, burp the child when it’s time to switch breasts and at the end of the feeding.
If it’s clear, however, that your baby isn’t spitting up much and really does not like it when you force him to stop for burping, it’s okay to wait until the he signals he’s had enough to eat.
To get those air bubbles up try one of these three positions:
- Put the baby on your shoulder.
- Sit the child up on your lap using a hand on the chest to support the chin.
- Lay the baby face down across your lap with the head raised slightly on your thigh.
Regardless of the position, the baby’s head should be just a little higher than the stomach.
Rub the baby’s back with your fingertips or palm. If the child is on your shoulder gently “dance” with the infant.
Generally after 4-5 minutes if a child hasn’t burped he doesn’t need to and you can stop trying.
After age 2-3 months, the child no longer needs to be burped regularly since it’s now spending more time in an upright position and awake. Under these circumstances, your baby will burp unassisted.
Want to read the entire thing?