CHAPTERS
Navigate to chapter
► Chapter 1: What’s Making Me Sneeze
► Chapter 2: Diagnosing and Treating Sinusitis
► Chapter 3: The Challenge of Chronic Sinusitis
► Chapter 4: Lifestyle and Alternative Therapies
► Chapter 5: Frequently Asked Questions
Chapter 1: What’s Making Me Sneeze
The real problem with sinus “problems” is how easily the symptoms they cause are confused with those of the common cold or allergies (seasonal and environmental). Depending on which nasal cavities are involved, you might even be diagnosed with migraines.
Long-term, chronic sinus problems adversely affect the lives of millions of people each year, causing pain, insomnia, fatigue, and an overall diminishment in the sufferer’s ability to enjoy life.
Sinusitis causes people to limit their leisure activities, like playing sports, and it raises the potential for life-long addiction to nose sprays and other “remedies.”
In the United States sinusitis is more common than heart disease. In 2004, the U.S. Centers for Disease Control and Prevention published a report indicating 35 million adults battle some degree of sinusitis every year, missing an aggregate 25 million workdays as a result.
At the same time, however, Americans dole out about $200 million annually on over-the-counter and prescription medications in an effort to get their sinuses back in good working order.
Sinusitis, Hay Fever and Allergic Rhinitis
From the beginning, it’s important to clarify these terms, which are often used interchangeably. They all refer to groups of symptoms affecting the nose and nasal passages. For the most part, we will be using the blanket term “sinusitis,” but let’s look at each one in turn.
What is Sinusitis?
In the simplest terms, sinusitis is an inflammation of the sinuses. There is, however, nothing simple about a condition that, in its short-term, acute phase resolves in a few weeks, but as a chronic problem may exhibit symptoms that fall up and down a broad spectrum of sinus-related secondary illnesses.
Unlike the common cold, which is caused by a virus, the culprit in triggering a bout of sinusitis is a one or more bacterium present in the respiratory system.
Sometimes you will see this same condition referred to as rhinosinusitis since both the nose and sinuses are often affected.
Adults age 20-65 are the most likely population to be confronted with sinus problems. Sinusitis is no respecter of persons, however, occurring equally among men and women.
Hay Fever and Allergic Rhinitis
“Hay fever” is the common term for allergic rhinitis. When a person breathes in dust or pollen to which they are allergic, the mucous membranes in the eyes and nose become inflamed and itchy.
This results in a runny nose and watery eyes, which can occur seasonally when a particular plant is pollinating, or be present year round with the reaction dependent on exposure.
People with hay fever in the spring tend to be sensitive to tree pollens, while summer allergies are generally to grass and weeds. In the fall of the year, weeds and fungus spores are the culprits.
When hay fever seems to be a year-round constant, the allergens are typically things that are present indoors like dust, feather bedding, carpeting, or animal dander. Mold in damp areas like basements and bathrooms can also be to blame.
The Perfect Nasal “Storm”
Because hay fever or allergic rhinitis leads to an inflammation of the mucous membranes, these conditions cause swelling in the nasal cavity and sinuses.
When the openings of the nasal cavities become blocked, a breeding ground for bacteria is created and infection can set in. The reason these conditions are discussed together is because of this intimate – and miserable – relationship.
While allergy treatments won’t cure a sinus infection, controlling allergies can stave off such an episode. Allergies aren’t themselves infections, but they create one of the many doors through which infection can enter.
The Human Nasal System
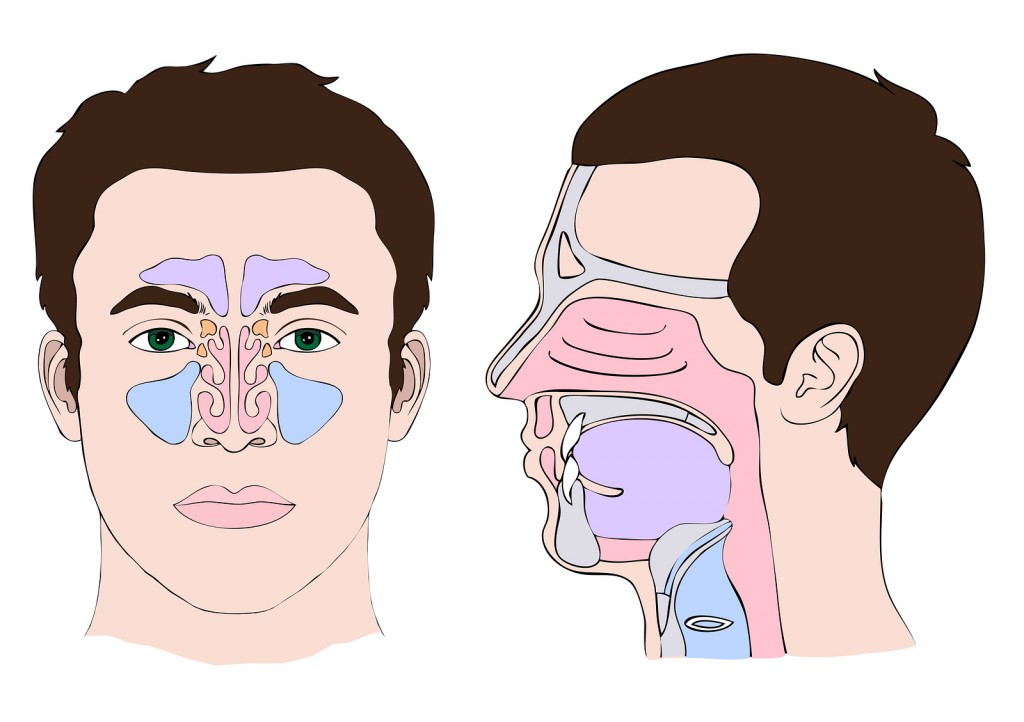
To understand the nature of the problem, it’s important to get a clear picture of how sinuses actually function in the human body.
We think of our nose as being our most prominent and obvious facial structure. It allows us to draw air into our lungs and to exhale carbon dioxide.
Most of us have some vague sense of where our sinuses are located, but little if any understanding of the intricate system involved in taking a single breath and preparing that air to reach the lungs in optimal condition.
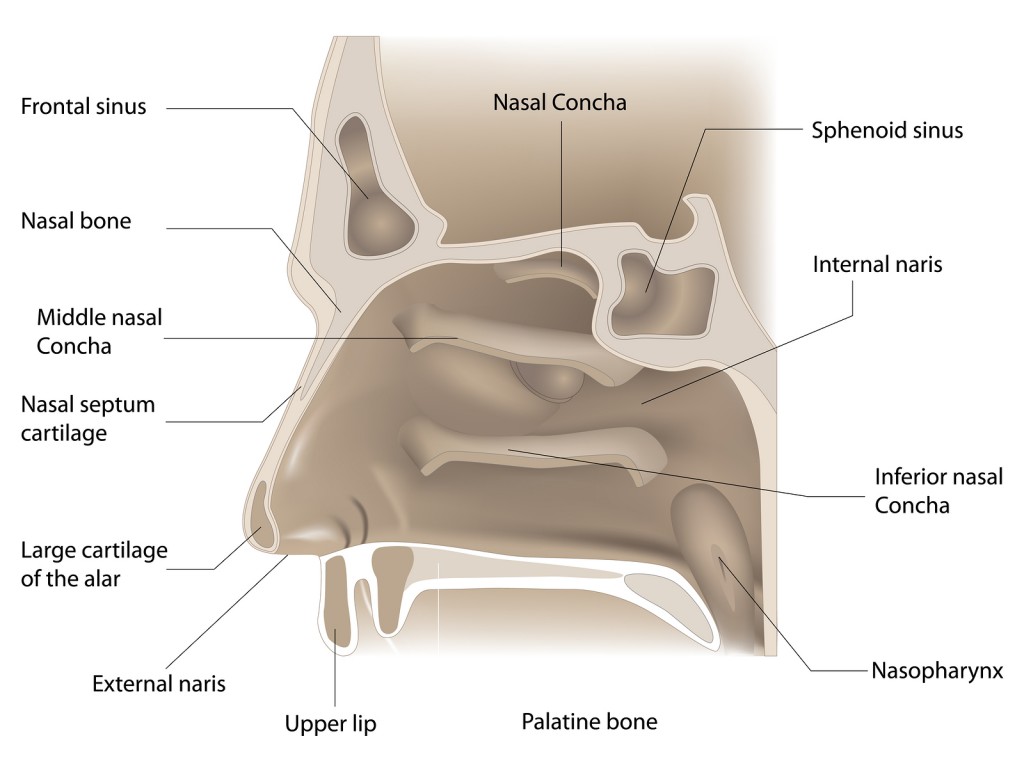
Structure of the Nose
The human nose is comprised of a soft tip made of cartilage, and a hard bridge made of bone. In between is an area called the nasal valve, which collapses inward when we take a deep breath.
The width of the nasal valve varies from person to person, and can itself be the cause of breathing issues.
On the interior of the nose between each nostril there is a thin wall of flexible cartilage called the septum. It progresses 3-4 inches back into the head and becomes solid bone along the way.
Nasal Cavity
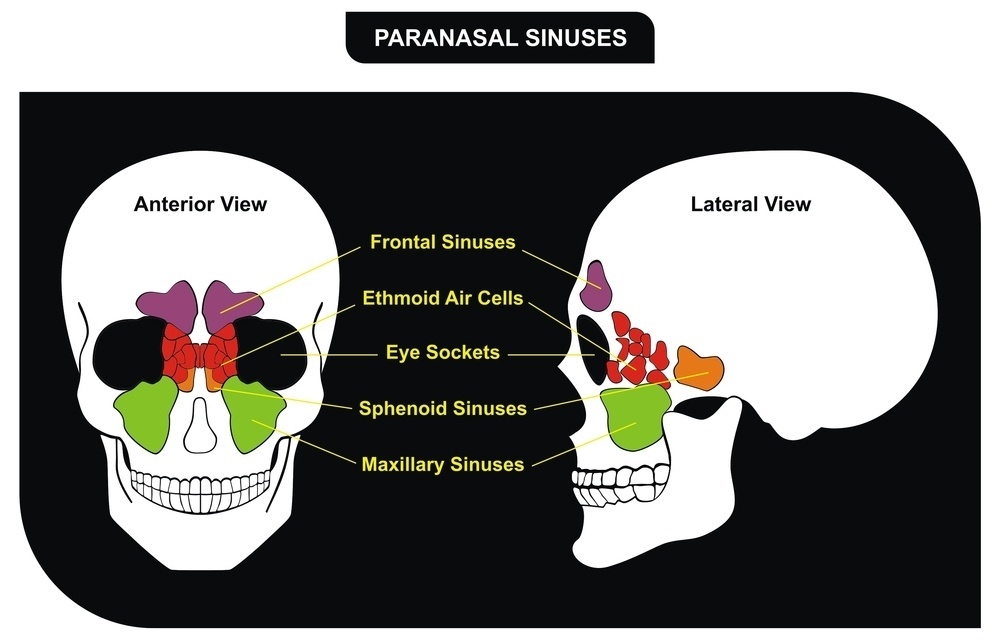
The nose leads to a region called the nasal cavity in which a series of openings called ostia adjoining four pairs of sinuses:
– maxillary – in the cheeks
– ethmoid – between the eyes
– frontal – in the forehead
– sphenoid – behind the nose
When the sinuses are healthy, the ostia are open, allowing air to flow freely in and mucus to drain out. If there is a problem, like swelling from an infection, the ostia close off and pressure builds up in the sinus.
The Turbinates
Humans can breathe through both their nose and mouth, but the nose is designed to both filter and warm the air we take in on its way to our lungs.
There are three sets of large bones behind the nose called the turbinates. The largest pair, the inferior turbinates, is at the bottom, roughly in a line with the base of the nostrils. They are approximately three inches in length.
On the next level up we find the slightly smaller middle turbinates (about 1.5 inches), and then the superior turbinates on top (an inch or less), roughly anterior to the bridge of the nose.
The turbinates circulate blood through their spongy, membranous surface to warm the air drawn in through the nostrils. Every six hours the volume of the blood flow in these surfaces switch sides as part of the nasal cycle.
If you have ever been aware of being able to breathe out of only one side of your nose, this is the normal functioning of the nasal cycle.
It switches back and forth throughout the day and night, but for the most part we are not aware of the change unless we consciously stop to check the air flow.
The air that comes into the nose and passes over the turbinates also picks up microscopic drops of moisture to improve its humidity level.
If you stand in front of a mirror and breathe on to the surface, the fog your breath creates illustrates the presence of this moisture in your nose.
Finally, the turbinates act as filters. The structures are covered in mucus that traps particles in the air we inhale and stops them from entering the lungs.
Ostiometal Complex
Before air reaches the sinuses, however, it must pass through the ostiomeatal complex, an area adjacent to the turbinates. Blockage of this structure is one of the most common triggers for an episode of sinusitis.
A Closer Look at the Sinuses
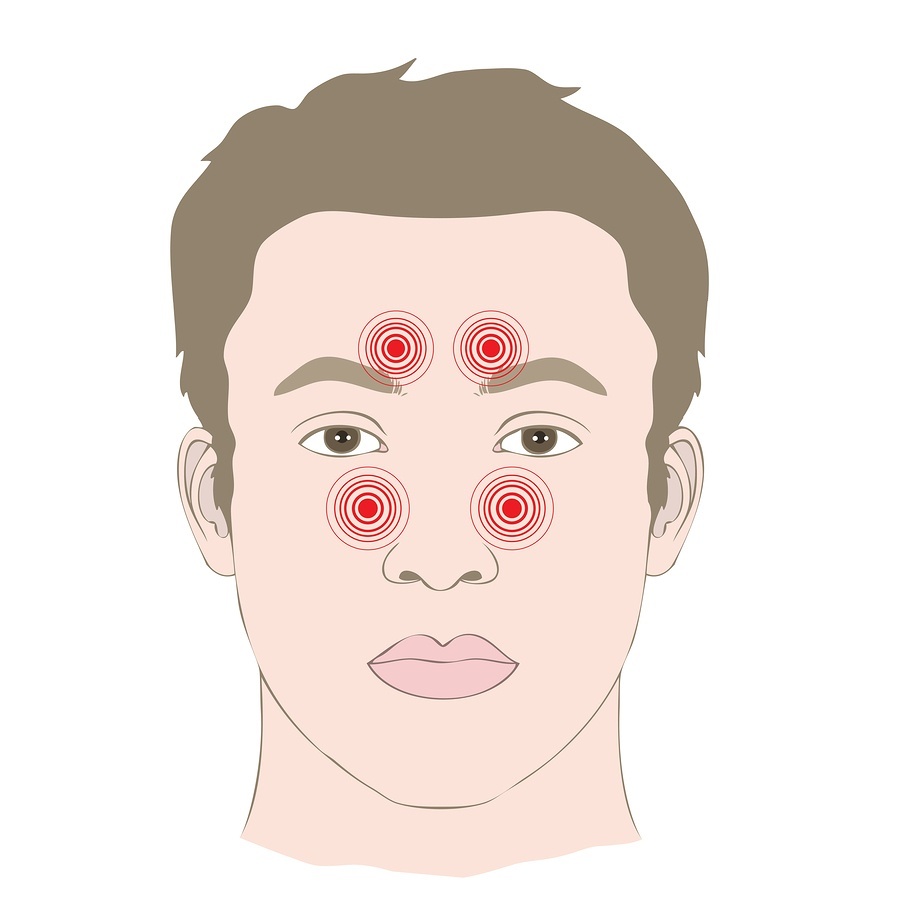
Pain and congestion can be present in each of the four pairs of sinuses or in combinations of these structures. This is why blocked ethmoid sinuses behind the eyes may be mistaken for a migraine, or issues with the maxillary sinuses may be wrongly diagnosed as a toothache.
Ethmoid Sinuses
The ethmoid sinuses are positioned between the eyes behind the bridge of the nose. They play a key role in the overall system of sinuses because the frontal and maxillary sinuses drain through them. If the ethmoids are not clear, the other sinuses will quickly become blocked as well.
The ethmoids are not single chambered, but are made up of 5-10 smaller chambers separated by thin walls covered with mucous membranes. The entire structure, however, is quite small, roughly the size of a matchbox.
Maxillary Sinuses
The maxillary sinuses are located in the cheeks. If they sit low enough, the roots of the upper teeth extend into the cavity’s floor. This is why some people experience upper tooth pain from a sinus infection.
The maxillary sinuses are triangular in configuration. Each one is roughly the size or a walnut.
Frontal Sinuses
If the frontal sinuses are present, they are located in the forehead between the eyes. About 90% of the population develops these sinuses.
The back wall of the frontal sinus is part of the bone that covers the brain. The size of the sinuses varies widely from person to person.
Sphenoid Sinuses
The deeply placed sphenoid sinuses are to the rear of the nose at the point where the eyes connect with the brain. They are about the size and shape of grapes.
The carotid artery runs through the outer walls of the sphenoid sinus and is sometimes visible when a physician is examining the area during surgery.
Internal Structure of the Sinuses
The surface of each of the sinus cavities is covered in small, bumpy glands that secrete mucus as well as a carpet of tiny hairs called cilia.
The sticky mucus serves to trap foreign particles and bacteria, while the cilia sweep the material away through the sinus opening and into the nose. The little hairs beat about six times a second and are very strong in relation to their size.
For instance, in order to push mucus through the ostia of the maxillary sinuses, the cilia actually have to overcome the force of gravity and move the material up to the opening.
This highly efficient process of mucociliary clearance moves approximately eight ounces of mucus a day through healthy sinuses.
Why Do We Have Sinuses?
In truth, there is no definite answer to the question of why human beings have sinuses. Without question, these empty spaces make the human head lighter, and thus may be an evolutionary adaptation to walking upright.
The structures also protect the eyes and brain by lessening the impact of blows to the face and head. They also make the structure of the skull less complicated so the facial bones can mature at an equal rate with the brain inside the cranial cavity.
These are not the only benefits derived from the sinuses, however. They improve our ability to taste and smell and provide resonance to the human voice.
The sinuses help to equalize pressure inside the nasal cavity and help to regulate our body temperature. Their filtering function is important to keep potentially harmful particles out of the lungs, and to ensure that the air we breathe is properly hydrated.
In fact, this whole system is a marvel of engineering efficiency as long as it’s open and functioning. When something goes wrong, however, the consequences for the individual can be absolutely miserable.
In studies conducted at the Harvard Medical School, people with chronic sinusitis reported higher levels of ongoing pain and discomfort than those patients dealing with chronic neck and lower back pain and even heart disease.
What Causes Sinusitis?
There are many potential causes for sinusitis, but one of the most common is an obstruction of the ostiomeatal complex adjacent to the turbinate bones.
This causes mucus to back up into the sinuses, which shuts down the action of the cilia. The mucous glands, however, continue to do their job even though the “drain” is clogged.
Remember that the interior of the sinus is an area that is both moist and warm, making it a natural breeding ground for bacteria. Normally the bacteria that inhabit the area are perfectly safe.
However, when the sinuses back up and the mucus becomes stagnant and foreign debris is not being removed, harmful bacteria begin to rapidly proliferate until infection sets in.
Your Body’s Response to Infection
Once that occurs, your body’s defensive mechanisms are activated. The human immune response, which is attempting to protect you from the infection, is a large part of what makes you so miserable with full-blown sinusitis.
The mucous glands begin to work even harder, churning out vast amounts of mucus and swelling with blood to fight the bacterial invasion.
White blood cells rush to the membranous lining with the intent of destroying the bacteria. Basically your body has gone to war, and the battlegrounds are tiny spaces in your head that rapidly become filled to capacity.
The results are headaches, an awful feeling of pressure, thick mucus that sludges down the back of your throat, irritating the lining and causing even more discomfort.
You can’t sleep at night. You can’t concentrate by day. You feel awful. All because your body is doing exactly what it’s supposed to do!
The longer the war goes on, the worse it tends to get. More of the sinuses become inflamed. There’s more swelling, more blockage, more bacteria — welcome to the “sinusitis cycle.” Now, what do you do about it?
Chapter 2: Diagnosing and Treating Sinusitis
Although the symptoms of sinusitis are fairly straightforward, they can present concurrently with other conditions often leading to repetitive misdiagnosis.
Allergic rhinitis is one of those conditions. It is all too common for a doctor to put a patient through a round of allergy treatments that may, in fact, only serve to make their symptoms worse. If an infection is the underlying cause of the sinusitis, that must be addressed.
The more you understand about the often-stubborn sinusitis “complex,” the more effectively you can participate in your own program of recovery.
Major Sinusitis Symptoms
There are three major symptoms of sinusitis that make the condition often unbearable for the person suffering through a flare up.
– pressure / pain
– difficulty breathing due to congestion
– post-nasal drip / sore throat
Treating and resolving these symptoms is the challenge of breaking the sinusitis cycle.
Pressure and Pain
Pain from an attack of sinusitis presents with a throbbing, dull ache. Swelling in the inflamed sinus puts pressure on the nerve endings in the sinus lining. Where you feel the discomfort depends entirely on the location of the affected sinus.
– If the inflammation is present in the frontal sinus, you will have a headache, typically centered in the forehead with an accompanying feeling of tightness.
– Affected maxillary sinuses make your face hurt, with the pain often radiating into the upper jaw as if you were suffering from a toothache.
– When the condition strikes the ethmoid sinus the pain is in the bridge of the nose and between the eyes.
– Sphenoid sinuses cause pain behind the eyes and at the top and base of the head.
A single set of sinuses may be involved in an attack of sinusitis or all of the passages can be affected. If this is the case, the condition is referred to as pansinusitis.
Congestion and Difficulty Breathing
Over-production of mucus in combination with swollen membranes further narrows the breathing passages on one or both sides of the nose.
This congestion may just be an inability to draw air in freely, or it may be a painful sense of fullness and pressure. Some sinus sufferers say their head feels heavy or seems “too big.”
If the ostia swell completely closed, the mucous membranes begin to absorb oxygen. This creates a vacuum which is even more painful.
Postnasal Drip and Sore Throat
Although mucus normally drains down the back of the throat, it is sufficiently thin that we don’t notice it’s there.
In the case of an infection, however, the mucus becomes thick and collects in the back of the throat, even pooling around the vocal cords.
This is why sufferers often wake up with a sore throat and a hacking cough until they can dislodge the mucus and cough it up.
High concentrations of white blood cells are present in this mucus, which irritate the lining of the throat. It is not at all uncommon for there to be excessive mucous discharge from the front of the nose as well.
Other Potential Symptoms
In addition to the three major symptoms of sinusitis, you may also experience:
– A diminished capacity to smell, which often accounts for the loss of appetite people experience during a bout of sinusitis.
– A concurrent lessening of the ability to taste. The human capacity to taste foods is dependent on smell. The loss of these two senses go hand in hand.
– Halitosis or bad breath caused by the bacteria present in the mucus drainage.
– Coughing as a measure to get rid of collected mucus in the back of the throat.
– Fatigue. In addition to the amount of energy your body is expending to fight the sinus infection, the symptoms of sinusitis make it almost impossible to get a good night’s sleep.
– A sense of fullness in the ears due to blockages of the Eustachian tube, which connects to the ears to the back of the nose.
– A fever as part of the body’s immunological response to the presence of the infection.
When people say that it’s sometimes impossible to function well with a case of sinusitis, they are not exaggerating!
Difficulties in Diagnosis
The principle difficulty in diagnosing sinusitis is the similarity of symptoms to those present with colds and allergies. It is also possible for an attack of sinusitis to begin with either of these events.
The Common Cold and Allergic Rhinitis
It’s important to realize that a virus causes the common cold, while bacteria triggers sinusitis. On average, a cold resolves in a week
Irritants in the environment cause allergies. They may be seasonal, or tied to instances of exposure to a substance to which the individual is sensitive (perennial).
Colds sometimes present with facial pressure and nasal discharge, but the mucus will be either thick and white or watery. If the mucus is from a sinus infection, it will be thick and greenish yellow.
Colds do not cause bad breath, but they do put the sufferer through coughing, sneezing, congestion, sore throat, and fatigue.
Nasal discharge from an allergy is clear, watery, and thin. Unlike either sinusitis or a cold, the person’ eyes will itch. There will be no bad breath.
Sneezing will definitely be present, but congestion, coughing, and sore throat vary widely by individual.
In all cases, if the symptoms last for more than a week, a visit to your primary care physician is in order.
Visiting Your Doctor
When you see your doctor, the first step toward a diagnosis will be gathering information for a patient history. This process also involves excluding other conditions that might be responsible for your symptoms.
For instance, facial pain in the absence of congestion might indicate a neurological illness like neuralgia.
As a diagnostic tool, your doctor will look into the front of the nose using a small flashlight to illuminate the visible portions of the inferior turbinates to look for swelling and signs of infection.
Some doctors will tap on the forehead and cheeks looking for indications of tenderness, but this is actually not a reliable method to check for sinusitis.
X-Rays or CT Scan?
At one time, taking an x-ray of the sinuses was regarded as the most reliable test to determine the presence of sinusitis.
On an x-ray, bones show up as white, empty spaces as black, and other structures, including a sinus packed with mucous, appear in gray.
X-rays have been replaced by CT scans, however, as the best way to determine the presence of sinusitis.
CT scans use a series of x-rays that image 1-3 mm “slices,” which are then assembled to give your doctor a 3D view of what’s going on in your nose and sinuses.
The procedure is completely painless and quite fast, taking less than 5 minutes. There are two variations of the test: limited and full.
Of the two, a limited scan is less expensive and tends to be the type most often ordered by primary care physicians. For a simple case of sinusitis this test will be sufficient.
If, however, you are referred to an ENT (ear / nose/ throat) doctor with a particularly stubborn case of sinusitis, you will likely be asked to have a second, full scan performed.
This will allow the doctor to more thoroughly diagnose the cause of the ongoing discomfort.
First Line Treatment
At the level of treatment you will receive from a primary care physician, you will likely be prescribed an antibiotic, and given advice on selecting an over-the-counter decongestant.
In a large number of cases, these measures will be sufficient to resolve an isolated case of sinusitis. If you have three or more episodes of sinusitis in any 12-month period, you will likely be referred to an ENT.
ENTs or otolaryngologists have specialized training and greater expertise in resolving persistent and chronic cases of sinusitis. Unlike primary care physicians, ENTs try to isolate the specific bacteria present, and look for and address physical abnormalities in the nasal cavity.
Referral to an ENT
If you are referred to an ENT, be prepared to go through your medical history again. Don’t be impatient with this process. Every doctor needs to work his own diagnostic procedure and an ENT will likely ask much more detailed questions.
Endoscopic Examination
In all likelihood the doctor will start with a visual examination of your nose using a nasal speculum to gently widen your nostrils for better access.
Next, he may progress to an endoscopic exam using a high-resolution camera on a thin stem. The end of the instrument that enters your nasal cavity is lighted, and the opposite end is outfitted with an eyepiece through which the doctor views the area.
In preparation to insert the instrument, you’ll receive a dose of a nasal decongestant spray and a mild topical anesthetic.
An endoscopic procedure doesn’t hurt, but it does create a tickling sensation that makes it hard for the patient to sit still, which is necessary for the doctor to be able to get a good look inside your nose.
Using the endoscope, the doctor will look for inflammation of the mucous membranes and check the meatus for signs of infection and turbinate enlargement. It may also be possible for him to see any polyps that are further blocking the sinuses.
Nasal Polyps and Cysts
Both nasal polyps and cysts are quite commonly revealed during CT scans and endoscopic examinations. Neither is cause for undue concern.
Cysts in the sinuses are filled with mucus and normally reach the size of a grape. They are typically quite harmless, and simply develop when a mucous gland becomes blocked.
Cysts occur most frequently in the maxillary sinuses.
When a cyst grows to its maximum size, it ruptures spontaneously and the mucus drains out. Most people have no idea this has even occurred, although they might notice a brief salty taste in their mouths. Very rarely does a cyst grow large enough that it requires surgical removal.
Polyps are growths roughly equal to the size of a pea. They grow on stalks emanating from the wall of the sinus and are common in people with chronically inflamed mucosa.
As the polyp grows, it can narrow the nasal passage causing congestion. Ultimately a polyp can completely block a sinus, triggering an overgrowth of bacteria and the development of sinusitis.
These growths rarely present as malignancies. It may be possible to shrink a polyp with the use of steroids, avoiding surgical removal.
Nasal Tumors
Any time a person is diagnosed with a growth of any sort, the mind naturally runs to one word “cancer.” It’s important to understand that nasal tumors are extremely rare. Polyps are not tumors.
When tumors do occur in the nasal passages, they are typically benign. Additionally, since the growths block the nose and cause sinusitis, they are detected early and easily removed.
If a nasal tumor was undetected, or allowed to grow quite large, it could certainly do a great deal of damage, but this rarely occurs.
Discovering Allergic Rhinitis
An endoscopic examination may also reveal swelling of the turbinates, especially the inferior turbinates. If this is the case, the greater sinus issue may actually be allergic rhinitis caused by environmental irritants that cause the nasal passages to swell.
Although the symptoms of allergic rhinitis are much the same as those of sinusitis, a CT scan may show that the sinuses are open.
Additional Testing
Depending on what your doctor sees through the endoscope, a full CT scan will likely be the next test ordered.
This could be followed by allergy testing or by a culture of the bacteria present in the nose. An MRI will not be ordered because an MRI works best to reveal details in soft tissue, not bony structures.
If a culture is performed, the swab will likely be taken using the endoscope again so the bacteria are obtained from the most seriously affected area. This will guide the doctor in prescribing the correct antibiotic.
Blood tests are also possible if your doctor believes that your sinus pain is linked to a larger systemic problem.
The Diagnosis
At this stage of combating your sinus problems, you will either be diagnosed with acute or chronic sinusitis. The only difference in the two labels is duration.
In a case of acute sinusitis, the symptoms resolve in 1-3 months. With chronic sinusitis, the symptoms last longer than three months.
Physiologically the only difference in the two diagnoses is that patients with acute sinusitis are more likely to have a fever.
If you are found to suffer from chronic sinusitis, you have a running battle on your hands, one where relapses are quite common.
Your quality of life will be affected to some degree, and finding the right combination of treatments to offer relief is more challenging.
Understanding Acute Sinusitis
In about 5% of cases, an episode of acute sinusitis is preceded by a cold. This progression is most likely in people who have naturally narrow sinus openings.
During the cold, sinus drainage becomes impaired and the area swells, leading to a backing up of the mucus and a proliferation of bacteria.
Although the cold itself is caused by any one of several rhinoviruses, the secondary sinus infection will be touched off by one of three common bacteria:
– Streptococcus pneumonia
– Haemophilus influenza
– Moraxella catarrhalis
Typically, a secondary infection is more persistent and harder to “kick” than the original cold.
Treating Acute Sinusitis
Resolving a case of acute sinusitis while offering the patient some degree of physical relief involves the interplay of several treatment strategies.
Over-the-counter painkillers are useful for the headache and pressure that accompany a sinus infection. It doesn’t really matter which product you choose. Acetaminiphen, ibuprofen, and aspirin will all work depending on personal preference.
Staying well hydrated is crucial. Getting as much water in your system as possible will help to thin the mucus in your sinuses for more effective and faster drainage.
This process should also include nasal irrigation with a saline solution, and exposure to steam from almost any source ranging from a comforting bowl of soup to a long, hot shower.
Ice compresses can also help with facial pain. Retail pharmacies sell special gel masks that can be frozen multiple times. These products are especially good because they conform more directly to the facial features for better coverage.
Prescription Medications
Once a patient is diagnosed with acute sinusitis, an ENT will prescribe an antibiotic and probably a decongestant. Although penicillin was once the standard treatment, too many strains of bacteria have developed resistance to the drug.
Antibiotics
Currently, amoxicillin is the most-prescribed medication, although it, too, is proving to be ineffective in as many as 30% of cases. The use of augmentin, a combination of amoxicillin and clavulanate is growing more popular for this reason.
Other antibiotics that may be administered include:
– azithromycin
– clarithromycin
– telithromycin
– cefpodoxime
– cefdinir
Axithromycin may be dispensed in a three-day course, commonly called a Tri-Pak, or as a five-day dosage, known as a Z-Pak.
The issue of decongestants is somewhat more complicated by how people use these medications on their own without a doctor’s guidance.
The Problem with Decongestants
Both your primary care physician and your ENT may recommend that you use a decongestant in the form of either an over-the-counter spray or tablet.
If you have chosen not to see your doctor and are dealing with your sinusitis alone, seeking relief from the pressure and congestion is one of the first things you’ll pursue.
Nasal Sprays and Rebound
Nasal sprays offer one of the most direct and instant means of relief for painful sinus congestion – almost too quick. With over-the-counter medications, people often think that if one dose is good, two is better.
Over-medicating with these items is common and dangerous. The implications for managing sinusitis are especially important.
The two active ingredients in most commercially available nasal decongestants are oxymetazoline or phenylephrine. Both cause a phenomenon called “rebound” if used for an extended period of time.
When rebound occurs, the swelling instantly returns when the effect of the spray wears off.
In fact, the swelling evident in rebound tends to be more severe, leading people to pick up the spray bottle and use even more of the preparation, seeking the same level of relief they initially received.
This sets up a vicious cycle of addiction, until the affected person literally cannot breathe for any extended period of time without a “hit” of nasal spray.
To avoid the development of rebound, a nasal spray with an active ingredient should never be used for more than 2-3 days.
A saline nasal spray can be used for any amount of time without fear of rebound, but these products do not deliver the same kind of dramatic results.
It is also a good idea to select a nasal spray that is formulated for mild doses of approximately four hours.
Regardless, only turn to a nasal spray to get yourself through really severe instances of congestion, otherwise, avoid these products.
Oral Decongestants
All oral decongestants have pseudoephedrine as their active ingredient. These pills are slower to provide relief from sinusitis, but they do not raise the potential for addictive rebound. They do, however, have other potentially harmful side effects.
People with high blood pressure should not use oral decongestants due to their propensity for causing heart palpitations.
Almost anyone can experience a sense of being “jittery” when taking pseudoephedrine, which can also cause insomnia.
Acute Sinusitis and Surgery
Thankfully in instances of acute sinusitis, surgery is almost never indicated unless the bacterial infection is so severe it actually breaks through a sinus wall.
If this were to occur, it would most likely happen in the ethmoid sinus where the intervening partitions are very thin.
Of those partitions, the lamina papyracea between the ethmoid sinus and the eye socket is the most vulnerable to perforations and abscesses.
Although rare, if this does occur, surgery is essential to drain the area and preserve vision.
Want to read the entire thing?